Choroidal Naevi: A Comprehensive Review and Insights into Current Therapeutics
Choroidal naevi are pigmented lesions that originate from the choroid, the vascular layer of the eye located under the retina. These are similar to pigmented spots or moles on the skin. These lesions occur in 5% to 10% of the general population. While the majority of choroidal naevi are asymptomatic and require no intervention, they may cause visual disturbances or exhibit concerning features such as orange pigment overlying the lesion or associated serious retinal detachment. They may also exhibit growth and features of malignant melanoma (i.e. cancer) that warrant close monitoring and potential treatment.
Clinical Presentation and Diagnosis
Choroidal naevi appear as well-defined, pigmented lesions with the formation of overlying deposits termed ‘drusen’ within the choroid. They can vary in size, color, and shape, ranging from small, flat lesions to larger, more elevated ones.
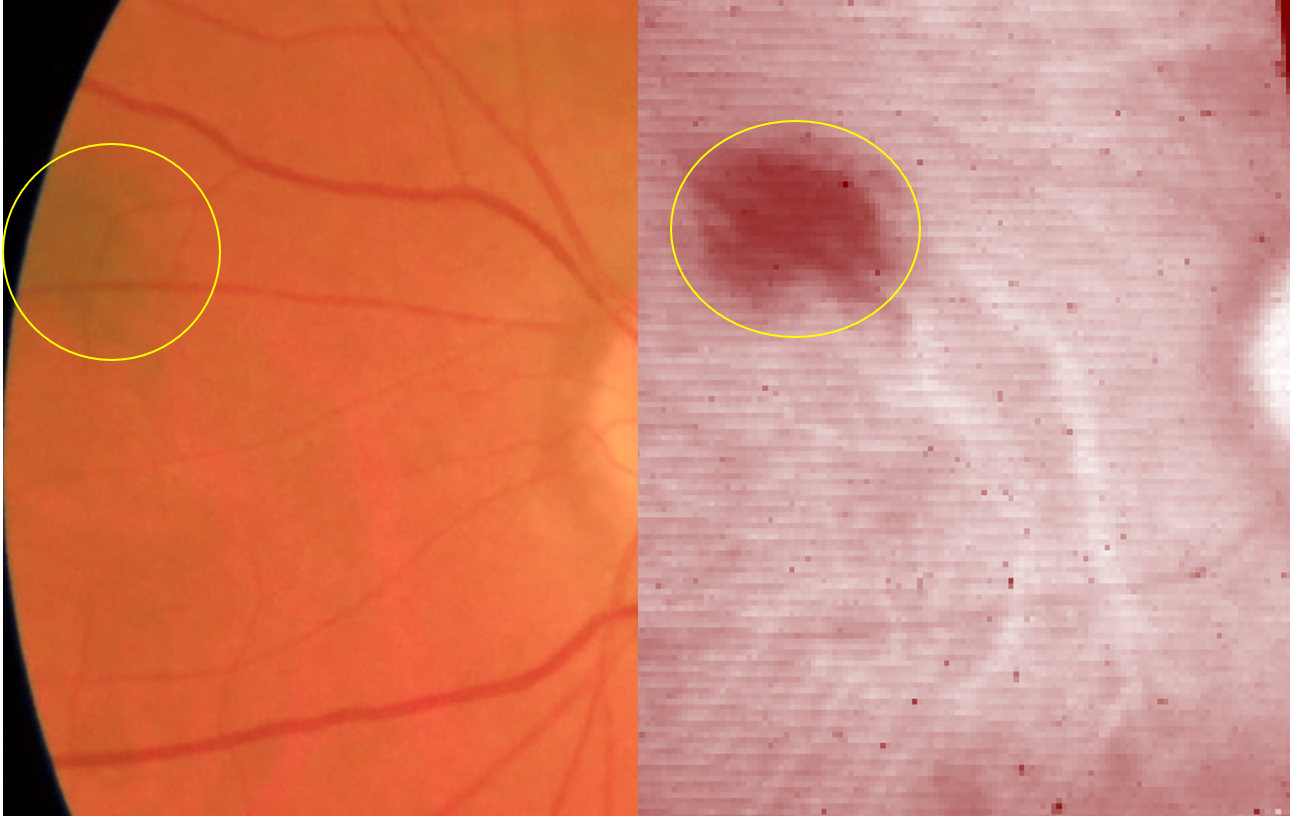
The possibility of developing into malignant melanomas makes their early and accurate characterisation necessary. Diagnostic techniques, such as fundus photography, optical coherence tomography (OCT), fluorescein angiography (FA), and indocyanine green angiography (ICGA) play crucial roles in the evaluation of these lesions. While these techniques are the current standard of care, they are costly and inaccessible to a vast majority.
Advancements in molecular genetic testing and techniques like hyperspectral retinal imaging (HSI) hold promise in providing novel insights into the signatures of choroidal naevi, facilitating more precise diagnosis and monitoring. Early detection and routine monitoring can be made cost efficient and accessible with hyperspectral retinal imaging.
Management and Therapeutics
Choroidal naevi are typically discovered during routine eye examinations. The majority of these are asymptomatic and require periodic monitoring to ensure there are no signs of growth or transformation. Factors that may increase the risk of tumor formation include the size of the lesion, the presence of subretinal fluid, and the location of the naevus within the eye.
However, in cases where the lesion exhibits cancer formation, further evaluation and potential treatment may be warranted. Techniques such as transpupillary thermotherapy (TTT) or photodynamic therapy (PDT) can be used to selectively treat the lesion while minimizing damage to surrounding healthy tissue.
Current management involves routine check-ups every 6 months to 3 years, straining healthcare systems and reducing accessibility for patients.Therefore, it is imperative to develop easily accessible diagnostic tools to enhance disease management and alleviate the strain on healthcare systems.
Emerging Therapies
Ongoing research is exploring the potential of novel therapeutic approaches for the management of choroidal naevi. These include the use of targeted molecular therapies, which have shown promise in the treatment of melanoma. Despite this, in serious cases of advanced metastatic melanomas survival rates as low as 28% at 2 years, 22% at 3 years, and 19% at 4 years are observed.
Additionally, the development of improved imaging modalities, such as hyperspectral retinal imaging imaging, may aid in the early detection and monitoring of choroidal naevi.
Conclusion
Choroidal naevi are common, benign pigmented lesions of the eye that typically require periodic monitoring. However, these lesions may exhibit concerning features that warrant development of malignant melanomas. The management of choroidal naevi involves a multidisciplinary approach, with a focus on early detection, close monitoring, and the selective use of surgical or emerging therapeutic interventions when necessary. Ongoing research in this field aims to improve our understanding of the natural history of choroidal naevi and develop more effective early detection strategies for timely detection and cost effective monitoring of those at risk of malignant transformation.
References:
Algazi, A. P., Tsai, K. K., Shoushtari, A. N., Munhoz, R. R., Eroglu, Z., Piulats, J. M., … & Carvajal, R. D. (2018). Clinical outcomes in metastatic uveal melanoma treated with PD-1 and PD-L1 antibodies. Cancer, 124(14), 2084-2092.
Ismail, R.K., Suijkarbuijk, K.P.M. et.al. (2022). Long-term survival of patients with advanced melanoma treated with BRAF-MEK inhibitors. Melanoma Resp, 32(6), 460–468.
Shields, C. L., Kaliki, S., Furuta, M., Fulco, E., Alarcon, C., & Shields, J. A. (2013). American Joint Committee on Cancer classification of posterior uveal melanoma (tumor size category) predicts prognosis in 7731 patients. Ophthalmology, 120(10), 2066-2071.
Shields, C. L., Kaliki, S., Livesey, M., Walker, B., Garoon, R., Bucci, M., & Shields, J. A. (2015). Association of ocular and oculodermal melanocytosis with the rate of uveal melanoma metastasis: analysis of 7872 consecutive eyes. JAMA Ophthalmology, 133(9), 1011-1018.
Shields, C. L., Furuta, M., Berman, E. L., Zahler, J. D., Hoberman, D. M., Dinh, D. H., … & Shields, J. A. (2009). Choroidal nevus transformation into melanoma: analysis of 2514 consecutive cases. Archives of Ophthalmology, 127(8), 981-987.
Shields, C. L., Furuta, M., Mashayekhi, A., Berman, E. L., Zahler, J. D., Hoberman, D. M., … & Shields, J. A. (2008). Clinical spectrum of choroidal nevi based on age at presentation in 3422 consecutive eyes. Ophthalmology, 115(3), 546-552.
Carvajal, R. D., Sosman, J. A., Quevedo, J. F., Milhem, M. M., Joshua, A. M., Kudchadkar, R. R., … & Schwartz, G. K. (2014). Effect of selumetinib vs chemotherapy on progression-free survival in uveal melanoma: a randomized clinical trial. JAMA, 311(23), 2397-2405.